Anatomy and Physiology
The arterial pulse may be palpated in the extremities and the neck. With the knowledge of the contour of these vessels, the operator may easily identify the location of the artery. The anatomy of every site of insertion must be analyzed to determine the landmarks, the depth, the relationship to adjacent anatomical structures, and the size of the artery.
The radial artery is superficial in the thenar area of the wrist where the radial bone joins the metacarpal bones. There, the radial pulse is best felt slightly medial to the extensor tendons of the thumb. The radial artery is a preferred site of insertion.
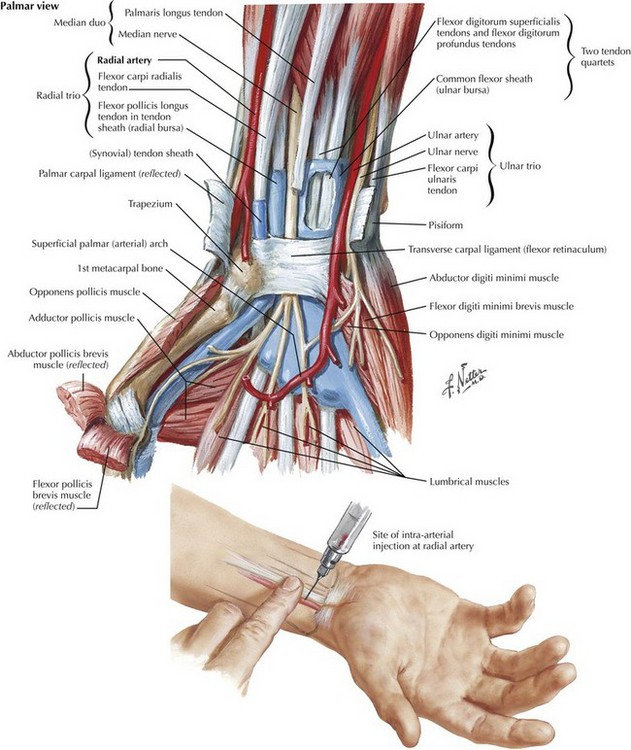
The ulnar artery is opposite to the radial pulse in the volar aspect of the wrist at the joint of the ulnar bone to the metacarpal bones. The artery divides into 2 branches, both of which join a similar division of the radial artery to form a rich, collateral network known as the deep and superficial palmar arch. The ulnar artery is smaller and not as readily palpable as the radial artery. It is used less commonly but may be accessed situations where other options have been exhausted.
The axillary artery rises to the superficial area of the axilla in its course through the pectoralis minor muscle which is delineated best while the arm is in the abduction. The pulsation of this large vessel can be palpated slightly lateral to the belly of the pectoralis major muscle into the axilla. The axillary vein hugs the artery very closely flowing on the medial aspect of the later. Both vessels are enveloped by branches of the brachial plexus as they all branch into different structures of the arm. The access and maintenance of the axillary artery require abduction of the arm. It may be used when peripheral options have failed. The axillary artery is near the thoracic wall and provides a central pressure waveform as it is advanced further into the subclavian artery.
The brachial approach of placing arterial catheters is traditionally considered problematic and prone to complication because of the paucity of arterial collateral circulation. It should not be accessed for cannulation to avoid the risk of ischemic injury to distal part of the extremity.
The pulse of the dorsalis pedis artery is readily felt on the bony prominence of the navicular bone at the mid-dorsal aspect of the foot. The operator reaches the artery as if performing a venipuncture aiming directly at the pulsation. There is ample collateral circulation of this artery making it a preferred access site of the lower extremity.
The posterior tibial artery is the second major arterial supply to the food running posterior to the medial malleolus in a groove that is bordered by the Achilles tendon posteriorly. There is a higher potential for occlusion of this artery because of its smaller caliber as compared to the dorsalis pedis artery.
The femoral artery gives the largest arterial supply of the lower extremity. The pulsation of this major vessel is a well-known landmark in juxtaposition to the femoral vein. The location of this pulse divides the inner third of the inguinal ligament to the outer two-thirds. The femoral artery is the single trunk that perfuses the lower extremity as it divides into 4 major branches as it wraps around the structures of the thigh. There are no other major collateral vessels for the arterial supply of the lower extremity. Therefore, complete obstruction of the femoral artery leading to ischemia may have devastating consequences.
The superficial temporal artery rises from the external carotid artery from the neck toward the temporal aspect of the skull anterior to the earlobe.
The umbilical artery can be visualized only for a few days after birth, while the umbilical stump has not yet involuted. A clean section of the umbilical stump readily displays 2 arteries and one larger thin-walled vessel representing the umbilical vein. During the first week after birth, the umbilical arteries are accessible, joining the iliac arteries respectively and the aortic artery subsequently.
Comments
Post a Comment